EULAR 2006 Odds and ends (posters):
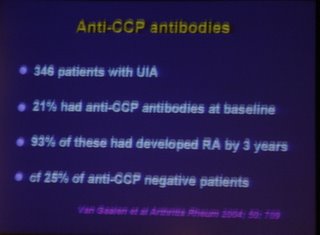
ESPOIR cohort: predicting the evolution of undifferentiated Inflammatory arthritis into RA. Multiple regression analysis gave the following odds ratios: Symmetrical onset 2.5; morning stiffness >60 minutes 1.7; synovitis >6 4.1; RF+ 2.2; anti-CCP+ 5.6. (Abstract THU0103). This does highlight the importance of anti-CCP. I hope we can get it soon.
Use of MTX (10-20mg/week) in Chronic pyrophosphate arthropathy. Tiny uncontrolled study of five patients but all reported as significantly improved. (THU0468)
Use of questionnaires to ask about recent medical and demographic events to improve efficiency in clinics (by T Pincus THU0130). I wonder if we should add something like this to our own clinic questionnaires?
Anti-CCP antibodies may predict which patients with palindromic rheumatism will evolve into RA (FRI0044). But what good that will do remains to be seen.
Patients on adalimumab seem to respond normally to immunisation against pneumococci and influenza (FRI0064). Which is I suppose useful.
Etanercept reported as effective in refractory PMR (series of 3, uncontrolled study) FRI0267. Significant changes in pain scores and HAQ of the order of 50%, but it only seemed to achieve a reduction in prednisolone of 5-7.5mg.
Two case reports of successful treatment of chronic tophaceous gout with infliximab. (FRI0491, FRI0496). Hmmm?
A Dutch study showed acute gout was more common in the Spring (FRI0495). I will mull over how that will change my practice.
A survey of UK rheumatologists (which included me!) showed that the BNF colchicine regime was used by only a minority. More than half used colchicine bd or tds.(FRI0498)
I have put the abstract numbers in, since you can get the abstracts online from the eular website http://www.eular.org
So what questions are raised by this meeting?

1. Can we be any better at predicting which patients with undifferentiated inflammatory arthritis will develop damaging arthritis?
Possibly, we know that anti-CCP positive patients with UIA are more likely to develop RA: 21% of UIA are CCP+, of those 93% develop RA, but 25% of CCP- also develop RA. In one talk this meeting it was suggested that a clinical prediction rule using 9 variables (including CCP) was able to assign patients such that only 6% of those predicted not to develop RA actually did go on to RA. This needs to be tested prospectively but if it does hold true, we need to consider if delaying treatment in this 6% with RA is acceptable. Clearly some members of the audience did not think it was. I will continue to treat all UIA/PISA with DMARDs for the time being.
I do wonder though if it might be feasible to use anti-CCP status to inform decisions about withdrawing DMARDs in that group which enters remission. They have either really gone into remission or are held in remission by treatment. It would seem reasonable to give greater consideration to stopping DMARDs in the CCP negative cases...but I do not think there is evidence to support this.
2. Which DMARD to use in early inflammatory arthritis?
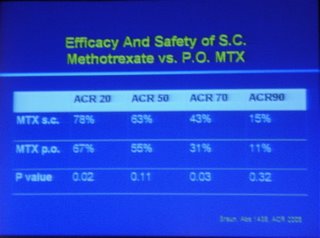
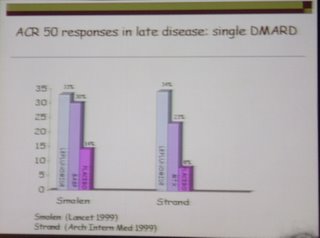
The easy answer is...one that works. But which to try first? If monotherapy is used it looks as if it should be with more intensive follow-up and tight control of synovitis (IM/IA steroids?). I tend to use MTX but the TICORA study did well with SASP as the initial drug.
MJM