Is the airway patent and protected? Guest podcast by Dr John Rutherford.
MP3 File
Sunday, December 31, 2006
Sunday, December 24, 2006
Wardround 22xii6

Merry Christmas!
Our two minute talks this week were on a favourite book/film/text, with relevence to medicine. I am pleased that this produced such an eclectic bag of goodies.
The choices were:
Jaws (Peter Benchley/Steven Spielberg): for, as Mark would have us believe, the inspiration to study shark attacks and develop a plan to manage such attacks.
The House of God (Samuel Shem): Before you walk a path, it is useful to read of those who went before. A must for all residents.
The Oxford Handbook of Clinical Medicine: A torch in the darkness (ignorance) of the first months of training. I am too old to have had one as a resident. Medical books were still in Latin back then. (Abite in malum rem).
My Sister’s Keeper (Jodi Picoult): for the ethical dilemmas. (A Richard and Judy recommendation, no less...so says Mrs Wardround).
Good Bye Lenin (Dir W Becker): truth and deception. Can deception, with the best of intentions, be right?
Scrubs: be presented with medical/ethical dilemmas disguised as comedy. Use as an aid when reflecting on your own actions and decisions...or those of others.
M*A*S*H: ditto.
MJM
Sunday, December 17, 2006
Wardround 15xii6

This week’s two minute talks were about emergencies: I have uploaded Dr Gunn’s summary sheet for anaphylaxis since it so impressed me.
A general learning point for all the emergencies is the need to consider the practicalities as well as the treatment. So get help quickly and put people to use as they show up (e.g. “put a line in the right arm, please”...”go and read the case notes”...”call the ITU consultant” etc). Know the doses of drugs you might need to use urgently. All the emergencies require the usual attention to ABCDE.
Sudden loss of consciousness (MR): get help, ABCDE, remember BM, rashes, OD.
Hypoglycaemia (MR): get help, ABCDE, remember unusual presentations: LOC, fits, TIA, blindness, apparently drunk. Be aware especially in those with chronic liver disease.
Anaphylaxis: get help, ABCDE, lots of fluids, oxygen, adrenaline, chlorpheniramine, steroids. 3mg of adrenaline is 3mls of 1:1000.
For next week’s talks we would like two minutes on your favourite book or film. The only caveat is that it must have a medical connection.
The paper for discussion on Tuesday is A field guide to experts.
Andrew D Oxman, Iain Chalmers, Alessandro Liberati.
BMJ 2004;329:1460-1463
Interesting topics
Pyrophosphate arthropathy
RS3PE
MJM
Sunday, December 10, 2006
Wardround 8xii6

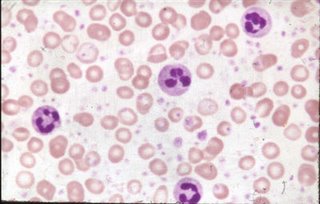
This week’s theme for two minute talks was Adverse Drug Reactions. ADRs are not uncommon and are sometimes fatal. Drug induced agranulocytosis mortality is shown in the figure. Even when an ADR is recognised, its presence may not be flagged up in the final diagnosis and the opportunity to prevent a repeat episode can be lost. When did you last write “Adverse Drug Reaction” in the diagnostic list?
In the talks we heard about:
Non-drug reactions (SS): the importance of asking patients if they are using non-prescribed remedies, the effects of food on drug activity such as pectins/digoxin and broccoli/warfarin.
Prevention (TJ): be aware of interactions with drugs you commonly use and check for interactions when the drug is unusual or has a narrow therapeutic window.
Diagnosis (HG)**: always consider ADR in your differential diagnoses. Be clear about information gathered and consider risk factors.
Warfarin and Antibiotics (RT): always check for interactions and monitor INR daily if interaction is expected. And of course, the second rule of ID, always ask yourself if the antibiotic is really needed.
Penicillins (AM): identify true allergy. Give some thought to the common situation of a patient reporting allergy to an antibiotic but not recalling which one. When you last prescribed an antibiotic did you tell the patient which one it was...or did you say “we’re giving you an antibiotic/a different antibiotic”
Amiodarone (MR): a bit of an aside here...MR, fight your corner, argue for your patient and don’t give in.
**=best talk
I was at a conference recently where one of the speakers had a paroxysm of acronymophilia while talking about ADRs. You will tell from the example that the example was an immunosuppressive agent.
S...Stratify: is the patient at higher risk of an ADR: comorbidities, drugs, age.
A...Assess: Hepatitis status, TB risk, vaccinations up to date?
F...Fend-off: vaccinate, optimise health (stop smoking etc).
E...Evaluate: check what ADRs might be expected, look for them.
T...Treat: nip it in the bud (UTI is easier to treat than septic multi-organ failure).
Y...Yearly: re-evaluate all of the above regularly. The frequency depends on the drug.
I have been contacted by EM from pharmacy, who has asked me to remind everyone about the risk of using ciprofloxacin in patients with epilepsy. And I will take the opportunity to mention the risk of ciprofloxacin in patients with tendonopathy (especially if on steroids). From a more general point of view we discussed the possibility of having a red dot system, similar to that used by radiographers, for the drug kardex. What do you think?
Next week’s two minute talks are on the OMG emergencies. We want to know the practical immediate management of:
Anaphylaxis (HG)
Hyperkalaemia (RT)
Sudden loss of consciousness (MR)
Hypoglycaemia (MR)
Sudden hypotension (TJ)
Sudden hypoxia (DK)
Two minutes please. Keep it concise yet precise and quote your sources. Can we make the handouts a visual aid? We don’t really need the talk written out.
The cardinal paper will be carried over once more...discussion on Tuesday as suggested by HG.
Interesting topics
Mitral regurgitation
ADR Agranulocytosis
Benign intracranial hypertension or alternatively
MJM
Saturday, December 09, 2006
Suspected PE
MP3 File
British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax 2003;58:470–484
Friday, December 01, 2006
Wardround 1xii6
This week’s two minute talk theme was common investigations. We heard about:
Rheumatoid factor (MJM): present in many inflammatory and infectious illnesses, more useful as a prognostic marker than in diagnosis, and a possible cause of interfernce with immunoassays.
D-dimer (PL) the physician’s bain – thought of as a “rule-out DVT test” by many but actually more of a “profiling the risk of DVT test”, has little practical application in patients who already have high pre-test probability of DVT.
Bilirubin (TJ) measurement may be influenced by food intake.
Glucose (AB): remember that venous and capillary samples give different results by as much as 1 mmol/l. Always get a lab sample at the extremes of results or where hypoglycaemia is suspected in a non-diabetic patient.
Troponin (HG): Excellent talk Dr Gunn: useful prognostic marker in ACIS but must be interpreted with other clinical variables.remember that haemolysed samples will give a spuriously low result. Remember that diseases other than ACIS can cause elevations of troponin and that the timing of the sample with respect to chest pain is important.
CRP (DK): a substance in the serum of patients with acute inflammation that reacted with the C polysaccharide of pneumococcus. Useful to monitor inflammatory activity in view of its short half life. CRP is associated with increased cardiovascular risk. (CRP <1mg/l>3mg/l =high risk).
Urinalysis (SS): have a look at the paper below in interesting topics.
We have deferred the paper for reading until next week. So for next week think about Hope is the thing with feathers. A piece of my mind, Cripe, LD. JAMA 296(15):1815-1816, October 18, 2006. Access it via the elibrary.
For next week’s two minute talks we are addressing adverse drug reactions:
Epidemiology (PA)
Diagnosis (HG)
Important drug interaction I (FY2)
Important drug Interaction II (FY1)
Improving safety (TJ)
Non-drug interactions (SS)
Two minutes only please. Be concise yet precise and quote your sources (not much of that this week). For the Important drug interaction talks choose an important example.
The combined wardround has fallen by the wayside (and been covered with Autumn leaves). It is time to get it going again. The round is difficult when an SHO has to leave at lunchtime so we should begin again (providing GAJ agrees?) on the following Fridays: 15th December, 5th January. Format to be agreed beforehand.
Interesting topics this week:
Rheumatoid factor (MJM): present in many inflammatory and infectious illnesses, more useful as a prognostic marker than in diagnosis, and a possible cause of interfernce with immunoassays.
D-dimer (PL) the physician’s bain – thought of as a “rule-out DVT test” by many but actually more of a “profiling the risk of DVT test”, has little practical application in patients who already have high pre-test probability of DVT.
Bilirubin (TJ) measurement may be influenced by food intake.
Glucose (AB): remember that venous and capillary samples give different results by as much as 1 mmol/l. Always get a lab sample at the extremes of results or where hypoglycaemia is suspected in a non-diabetic patient.
Troponin (HG): Excellent talk Dr Gunn: useful prognostic marker in ACIS but must be interpreted with other clinical variables.remember that haemolysed samples will give a spuriously low result. Remember that diseases other than ACIS can cause elevations of troponin and that the timing of the sample with respect to chest pain is important.
CRP (DK): a substance in the serum of patients with acute inflammation that reacted with the C polysaccharide of pneumococcus. Useful to monitor inflammatory activity in view of its short half life. CRP is associated with increased cardiovascular risk. (CRP <1mg/l>3mg/l =high risk).
Urinalysis (SS): have a look at the paper below in interesting topics.
We have deferred the paper for reading until next week. So for next week think about Hope is the thing with feathers. A piece of my mind, Cripe, LD. JAMA 296(15):1815-1816, October 18, 2006. Access it via the elibrary.
For next week’s two minute talks we are addressing adverse drug reactions:
Epidemiology (PA)
Diagnosis (HG)
Important drug interaction I (FY2)
Important drug Interaction II (FY1)
Improving safety (TJ)
Non-drug interactions (SS)
Two minutes only please. Be concise yet precise and quote your sources (not much of that this week). For the Important drug interaction talks choose an important example.
The combined wardround has fallen by the wayside (and been covered with Autumn leaves). It is time to get it going again. The round is difficult when an SHO has to leave at lunchtime so we should begin again (providing GAJ agrees?) on the following Fridays: 15th December, 5th January. Format to be agreed beforehand.
Interesting topics this week:
Sunday, November 26, 2006
Wardround 24xi6
This week's two minutes were themed about 'a patient who changed me/my practice'and with the discussion paper on end of life, turned into quite a discussion. It is useful to reflect on how we change our views as we gain experience and mature and the nature of professional versus societal responsibility.
Next week's two minute tutorials will be based on 'some common tests':
CRP (DK)
Troponin (HG)
D-dimer (PL)
Urinalysis (SS)
Keep it concise and precise.
The paper for reading is A PIECE OF MY MIND, Cripe, Larry D. JAMA 296(15):1815-1816, October 18, 2006. Access it via the elibrary.
Interesting topics
AION
Papilloedema
Drug rashes
MJM
Next week's two minute tutorials will be based on 'some common tests':
CRP (DK)
Troponin (HG)
D-dimer (PL)
Urinalysis (SS)
Keep it concise and precise.
The paper for reading is A PIECE OF MY MIND, Cripe, Larry D. JAMA 296(15):1815-1816, October 18, 2006. Access it via the elibrary.
Interesting topics
AION
Papilloedema
Drug rashes
MJM
Sunday, November 19, 2006
Wardround 17xi6
A brief blog, sorry.
This week we discussed alternative medicine. I would like to hold on to the concept from the professor of alternative medicine in Exeter: Alternative medicine (as opposed to conventional medicine) is a treatment that has not yet been shown (with scientific rigour) to be effective. By his definition a substantial part of conventional practice is 'alternative'. We should not forget that. I find the NCCAM website http://nccam.nih.gov/ a useful first port of call when a patient asks about a specific complementary treatment.
The read and think for next week will be Measuring quality of life. Is there such a thing as a life not worth living?
Bobbie Farsides, Robert J Dunlop BMJ 2001;322:1481-1483 ( 16 June ).
I had to leave before the end of the presentations this week so if you already have assignments for next week, do those. If not, let's have two minutes on "an episode which changed me/my practice".
MJM
This week we discussed alternative medicine. I would like to hold on to the concept from the professor of alternative medicine in Exeter: Alternative medicine (as opposed to conventional medicine) is a treatment that has not yet been shown (with scientific rigour) to be effective. By his definition a substantial part of conventional practice is 'alternative'. We should not forget that. I find the NCCAM website http://nccam.nih.gov/ a useful first port of call when a patient asks about a specific complementary treatment.
The read and think for next week will be Measuring quality of life. Is there such a thing as a life not worth living?
Bobbie Farsides, Robert J Dunlop BMJ 2001;322:1481-1483 ( 16 June ).
I had to leave before the end of the presentations this week so if you already have assignments for next week, do those. If not, let's have two minutes on "an episode which changed me/my practice".
MJM
Sunday, November 05, 2006
Wardround 3xi6
This week's two minute talks were on poisoning. We heard about paracetamol (PL), and the importance of early treatment, early liaison with the transplant unit, and factors which make toxicity more likely. I didn't realise that Gilbert's disease was included in this list. The talk on ethanol and methanol (JW) led us to discuss the early management of unexplained coma (ABCDE-BM). I like the idea of ethanol poisoning being a 'diagnosis of exclusion' but would recommend you have in your mind what you intend to eclude before accepting the diagnosis (true of every diagnosis of exclusion). Tri-cyclics (CC): I agree with Dr Jones that these are the most worrying of the common diagnoses. The watchword should be 'beware'. Be aware of vital signs, ECG (PR, QRS and QT), and acid-base status. Finally we came to carbon monoxide poisoning (AC), and AC raised an interesting point as to possibility of imcreasing oxygen deliverty with CPAP. Prize for the best talk goes to AC.
We had a chance to discuss the Bruno Sachs paper, which had a mixed response. I have to admit that despite trying quite hard I could not bring myself to like it. It did however kick off a discussion about the way we learn what might be called the social aspects of practice.
For next week's talks the theme is making decisions for patients, the legal aspects. Two minutes please on:
Adults with incapacity act (PL)
Emergency detantion orders (CC)
Short term detention orders (SS)
Compulsory treatment orders (AC)
PHA (JW)
Be concise and precise, and quote your sources.
Reading for next week: What's a good doctor and how do you make one? Hurwitz B et al , BMJ 2002;325:667-668
Interesting topics this week:
Tolosa-Hunt syndrome
HOCM
MJM
We had a chance to discuss the Bruno Sachs paper, which had a mixed response. I have to admit that despite trying quite hard I could not bring myself to like it. It did however kick off a discussion about the way we learn what might be called the social aspects of practice.
For next week's talks the theme is making decisions for patients, the legal aspects. Two minutes please on:
Adults with incapacity act (PL)
Emergency detantion orders (CC)
Short term detention orders (SS)
Compulsory treatment orders (AC)
PHA (JW)
Be concise and precise, and quote your sources.
Reading for next week: What's a good doctor and how do you make one? Hurwitz B et al , BMJ 2002;325:667-668
Interesting topics this week:
Tolosa-Hunt syndrome
HOCM
MJM
Sunday, October 29, 2006
Wardround 27x6
This week's theme for the two minute talks was ACIS. This stimulated enough discussion to shunt the discussion paper to next week. Troponin levels in patients on dialysis programs were raised and it has been suggested that their levels may be elevated..Have a look at this article. Hopefully we will be told the average troponins in these patients next week (or post it in the comments). You can also look at this article about changing rates of myocardial infarction. Could I ask you to post the NNts for treatment in the comments section.
The read and think for 3xi6 will be Dr Bruno Sachs addresses an audience of first year medical students: an extract from the writing of Martin Winckler, French doctor and writer
Med. Humanities 2006; 32: 1-3.
Next week's topic is poisoning: I have left my notebook (paper type) at work and can only recall one person's assignment...I can I am sure trust you to own up to which is yours.
Tricyclics
Carbon monoxide
Paracetamol
Ethanol and methanol (JW)
Interesting topics
Systemic rheumatoid vasculitis
A very recent review Systemic rheumatoid vasculitis: A review. Marcia S. Genta et al. Seminars in Arthritis and Rheumatism. October 2006, pages 88-98
MJM
The read and think for 3xi6 will be Dr Bruno Sachs addresses an audience of first year medical students: an extract from the writing of Martin Winckler, French doctor and writer
Med. Humanities 2006; 32: 1-3.
Next week's topic is poisoning: I have left my notebook (paper type) at work and can only recall one person's assignment...I can I am sure trust you to own up to which is yours.
Tricyclics
Carbon monoxide
Paracetamol
Ethanol and methanol (JW)
Interesting topics
Systemic rheumatoid vasculitis
A very recent review Systemic rheumatoid vasculitis: A review. Marcia S. Genta et al. Seminars in Arthritis and Rheumatism. October 2006, pages 88-98
MJM
Monday, October 23, 2006
Wardround 20x6
The Theme for next week's tutorials is ACIS. Could we have two minutes please on the role of each of the following in ACIS:
Investigation ()
Thrombolysis (SS)
Anti-platelet agents (CO)
'Intervention' (CC)
Beta blockers (DK)
I feel that the ratio of mumbling chatter to intellectual discussion is getting out of hand...so the two minutes starts promptly when I say "go". Give out your handouts before the talks start. Keep it precise and concise, don't tell us the obvious. Remember that Dr Thomas wants some NNTs. Don't forget the NNH though.
The read and think for 27x6 will be Dr Bruno Sachs addresses an audience of first year medical students: an extract from the writing of Martin Winckler, French doctor and writer
Med. Humanities 2006; 32: 1-3.
Interesting topics
Myoclonus
What does the pharmacist's symbol "Rx" mean?
MJM
Investigation ()
Thrombolysis (SS)
Anti-platelet agents (CO)
'Intervention' (CC)
Beta blockers (DK)
I feel that the ratio of mumbling chatter to intellectual discussion is getting out of hand...so the two minutes starts promptly when I say "go". Give out your handouts before the talks start. Keep it precise and concise, don't tell us the obvious. Remember that Dr Thomas wants some NNTs. Don't forget the NNH though.
The read and think for 27x6 will be Dr Bruno Sachs addresses an audience of first year medical students: an extract from the writing of Martin Winckler, French doctor and writer
Med. Humanities 2006; 32: 1-3.
Interesting topics
Myoclonus
What does the pharmacist's symbol "Rx" mean?
MJM
Monday, October 09, 2006
Wardround 6x6
Brief I'm afraid...to blog on holiday is to invite the family's wrath.
Next week's assignments:
Thrombocytopenia DK
Neutropenia SS
Lymphopenia CC
Pancytopenia ?
The reading is Diogenes syndrome
I'll be back after some R&R
MJM
Next week's assignments:
Thrombocytopenia DK
Neutropenia SS
Lymphopenia CC
Pancytopenia ?
The reading is Diogenes syndrome
I'll be back after some R&R
MJM
Monday, October 02, 2006
Wardround 29ix6
The theme for our tutorials this week was occupation related diease. I must say that I found this one of the most interestingsubjects we have done. Thank you to Dr Cameron for suggesting the subject. Perhaps everyone could post a one-liner about their particular subject, and advice on a source to read more, in the comments section? The prize this week toAC. I especially like the JAMA. 2006;296:1401-1404. I had rather mixed feelings about the paper. The discussion about the structure of an apology was perhaps useful but I was was a little concerned that an intervention such as this should be presented in such a positive way without the rigour (ie evidence for usefulness) usually attached to medical interventions. A ‘food for thought’; paper without doubt.
Next week we will address some practical problems faced by house officers. So two minutes please, concise and precise, on:
The confused patient (VJ)
Discharge against medical advice (AC)
The violent patient (DK)
‘The obs are fine but he’s just not right doctor’ (SS)
The paper for read and think is Mistakes. Ruth Lesnewski. JAMA. 2006;296:1327-1328.
Get the full text via elibrary
Interesting topics
Neurological problems due to B12 deficiency
MJM
Next week we will address some practical problems faced by house officers. So two minutes please, concise and precise, on:
The confused patient (VJ)
Discharge against medical advice (AC)
The violent patient (DK)
‘The obs are fine but he’s just not right doctor’ (SS)
The paper for read and think is Mistakes. Ruth Lesnewski. JAMA. 2006;296:1327-1328.
Get the full text via elibrary
Interesting topics
Neurological problems due to B12 deficiency
MJM
Monday, September 25, 2006
Wardround 23ix6

This week’s theme had been disorders which can mimic anxiety/panic attacks. We heard about phaeochromocytoma in an excellent talk from VJ Thyrotoxicosis, SVT, Hypoxia, prescription drugs and substances of abuse. My prize for the week goes to AC since he specifically compared the rates of symptoms in panic with the same symptoms in SVT. I would like to re-iterate my maxim that panic attacks do not exist in medical in-patients (pre-test probability low). Though the features of a panic attack (as per DSM IV) may well be present you should look hard for an alternative diagnosis. Be especially wary of findings which are not explained by panic alone.
The discussion paper was Does This Patient With Headache Have a Migraine or Need Neuroimaging? Michael E. Detsky et al JAMA. 2006;296:1274-1283. The conclusion of which was "The presence of 4 simple historical features can accurately diagnose migraine. Several individual clinical features were found to be associated with a significant intracranial abnormality, and patients with these features should undergo neuroimaging... The features are summarized by the mnemonic POUNDing (Pulsating, duration of 4-72 hOurs, Unilateral, Nausea, Disabling. If 4 of the 5 criteria are met, the likelihood ratio... for definite or possible migraine is 24."
In next week's two minute tutorials we will address occupational diseases:
Respiratory (VJ)
Neurological (AC)
GI/GU (s)
Musculoskeletal (CC)
Skin (MJM)
(and infections GAJ?)
Two minutes only, keep it concise and precise; quote your sources.
For the 29th I would like you to read and consider Apology in Medical Practice: An Emerging Clinical Skill. Aaron Lazare. JAMA. 2006;296:1401-1404.
Get the full text via library/elibrary.
Interesting topics
Acute sarcoidosis
MJM
Monday, September 18, 2006
Wardround 15ix6
The theme for this week was Venous thromboembolism. We heard from CC about the epidemiology of VTE (extrememly important given the need for pre-test probability assessments prior to lab testing); from VJ regarding investigation (the synthesis of clinical assessment such as Well’s with d-dimer estimation and imaging); and from AC about treatment. The prize this week goes to Dr Joshi for a well presented talk with excellent handout and quoted sources.
The discussion paper raised the importance of precision in diagnosis and communication. Investigations leading to a low probability of DVT are not the same as excluding DVT, even if the treatment decision is to not anticoagulate.
Next week’s theme is disorders which may present as ‘anxiety’:
Phaeochromocytoma (VJ)
Thyrotoxicosis
SVT (AC)
Hypoxia (CC)
Prescription Drugs (MJM)
Substance misuse (GAJ)
(we are not doing PTE since we have so recently done VTE)
wo minutes only, keep it concise and precise; quote your sources.
The paper for discussion on 22nd is Does This Patient With Headache Have a Migraine or Need Neuroimaging? Michael E. Detsky et al JAMA. 2006;296:1274-1283. Get it via the elibrary.
Interesting topics:
Retroperitoneal Fibrosis
The case for chocolate
MJM
The discussion paper raised the importance of precision in diagnosis and communication. Investigations leading to a low probability of DVT are not the same as excluding DVT, even if the treatment decision is to not anticoagulate.
Next week’s theme is disorders which may present as ‘anxiety’:
Phaeochromocytoma (VJ)
Thyrotoxicosis
SVT (AC)
Hypoxia (CC)
Prescription Drugs (MJM)
Substance misuse (GAJ)
(we are not doing PTE since we have so recently done VTE)
wo minutes only, keep it concise and precise; quote your sources.
The paper for discussion on 22nd is Does This Patient With Headache Have a Migraine or Need Neuroimaging? Michael E. Detsky et al JAMA. 2006;296:1274-1283. Get it via the elibrary.
Interesting topics:
Retroperitoneal Fibrosis
The case for chocolate
MJM
Friday, September 08, 2006
Wardround 8ix6
 This week’s discussions were disrupted by the ID team. No coincidence, I think, that the rheumatology discussion was subverted to ID. All part of the greater conspiracy? Next they will be claiming that rheumatoid arthritis is an infection.
This week’s discussions were disrupted by the ID team. No coincidence, I think, that the rheumatology discussion was subverted to ID. All part of the greater conspiracy? Next they will be claiming that rheumatoid arthritis is an infection.Perhaps those who did not have opportunity to present will post some brief comments? Dr Joshi’s exposition on the safe use of sulfasalazine was well designed and practical, especially his final paragraph about responding to problems.
We will have to discuss the homeless man on another occasion.
For next week I have chosen neutral ground, neither primarily ID nor Rheumatology: Venous thromboembolism…assignments as below, though you may swap uif you see fit. If your name does not appear you can still do two minutes on an aspect of VTE.
Epidemiology (CC)
Investigation (VJ)
Treatment (AC)
Prognosis
Remember, only two minutes...keep it concise yet precise...quote your sources.
The paper for discussion is from the parliamentary ombudsman and relates to case 200501128
Read and think….have something to say.
Interesting topics this week
Thrombocythaemia
HOCM
MJM
Sunday, September 03, 2006
Wardround 1ix6
The week's two minute talks were themed about antiviral treatment. Would each of you click the comment section and put in one sentence from your reading of the subject?
Next week we will hear about the safer use of DMARDs. The BSR last week published its guidelines for these drugs. You can get the local guidelines from my secretary. I had hoped to give a link to the BSR guideline but it has been taken off the website. I'll put in a link if it comes back. So we will hear about:
Methotrexate (CC)
Sulfasalazine (VJ)
Leflunomide (DL)
Etanercept (BW)
Next week's reading will be The homeless man on morning rounds. Jerome Lowenstein. I will leave a copy on the ward.
Interesting topics:
Homocysteine
Biventricular pacing
MJM
Next week we will hear about the safer use of DMARDs. The BSR last week published its guidelines for these drugs. You can get the local guidelines from my secretary. I had hoped to give a link to the BSR guideline but it has been taken off the website. I'll put in a link if it comes back. So we will hear about:
Methotrexate (CC)
Sulfasalazine (VJ)
Leflunomide (DL)
Etanercept (BW)
Next week's reading will be The homeless man on morning rounds. Jerome Lowenstein. I will leave a copy on the ward.
Interesting topics:
Homocysteine
Biventricular pacing
MJM
Sunday, August 27, 2006
Wardround 25viii6
This week’s two minute talks were themed around hospital acquired infection:
HA UTI (DL) and HA Pneumonia (BW), both were well researched and almost to time. Could I ask that next week you begin to list your sources so that others can follow up on reading.
For next week the theme will be anti-viral treatments, with assignments as follows:
Hepatitis C (BW)
Hepatitis B (?GAJ)
Herpes viruses (MJM)
Influenza (CC)
SARS (LD)
Keep to time, be concise but precise, and quote your sources.
The paper for discussion had been: Changing the Paradigm for HIV Testing — The End of Exceptionalism. Ronald Bayer, Amy L. Fairchild. NEJM August 17 2006, Volume 355:647-649. Apologies to everyone for my rather abrupt and dogmatic devil’s advocacy. The paper, though ostensibly about a specific ethical issue, does offer food for thought about informed consent in general. A study has been done in D&G surveying patient's views about consent in lab testing, so perhaps we can bring that along for discussion sometime?
For next week’s reading I thought we might have something clinical rather than ethical. So let’s give some thought to syncope. Read Current evaluation and management of syncope. Kapoor WN. Circulation, Sept 24, 2002;106 (13):1606-1609.
Interesting topics this week
Periodic fever
Herpes Encephalitis
Tilt testing
uptodate also has a good introductory article on the subject.
MJM
HA UTI (DL) and HA Pneumonia (BW), both were well researched and almost to time. Could I ask that next week you begin to list your sources so that others can follow up on reading.
For next week the theme will be anti-viral treatments, with assignments as follows:
Hepatitis C (BW)
Hepatitis B (?GAJ)
Herpes viruses (MJM)
Influenza (CC)
SARS (LD)
Keep to time, be concise but precise, and quote your sources.
The paper for discussion had been: Changing the Paradigm for HIV Testing — The End of Exceptionalism. Ronald Bayer, Amy L. Fairchild. NEJM August 17 2006, Volume 355:647-649. Apologies to everyone for my rather abrupt and dogmatic devil’s advocacy. The paper, though ostensibly about a specific ethical issue, does offer food for thought about informed consent in general. A study has been done in D&G surveying patient's views about consent in lab testing, so perhaps we can bring that along for discussion sometime?
For next week’s reading I thought we might have something clinical rather than ethical. So let’s give some thought to syncope. Read Current evaluation and management of syncope. Kapoor WN. Circulation, Sept 24, 2002;106 (13):1606-1609.
Interesting topics this week
Periodic fever
Herpes Encephalitis
Tilt testing
uptodate also has a good introductory article on the subject.
MJM
Friday, August 18, 2006
Wardround 18viii6
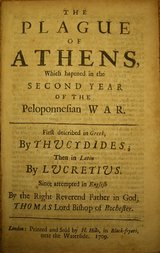
The reading for this week and the two minute talks were themed around the Plague of Athens. All well thought out with logical approaches to diagnosis. The internet is full of sites discussing the possible diagnoses, but you might find this article useful:
The cause of the plague of Athens: plague, typhoid, typhus, smallpox, or measles? Burke A. Cunha, Infect Dis Clin N Am 18 (2004) 29–43.
Now I know DL had difficulty getting these out of the eLibrary but I have tried again today and could access the PDFs without difficulty (except having to enter my athens password twice). Go on take the challenge…access this journal on-line. I have left a copy on the ward if you are unsuccessful. This copy of Infect Dis Clin N Am has a historical theme and the other articles are worth a look. I particularly liked:
Osler on typhoid fever: differentiating typhoid from typhus and malaria. Cunha BA. Dis Clin North Am. 2004 Mar;18(1):111-25.
Next week’s two minute tutorials are on hospital acquired infection:
Dr Mohan will be leaving us but those left behind can fight on. Hosp. acquired UTI (Dr Lindsay), Hospital Acquired pneumonia (Dr Williams). Two minutes please keep it concise and precise.
The reading for next week is for once quite up to date. Changing the Paradigm for HIV Testing — The End of Exceptionalism. Ronald Bayer, Amy L. Fairchild. NEJM August 17 2006, Volume 355:647-649. Read and think
Interesting topics this week
Arteritis
Hypokalaemia
Ankylosing spondylitis
Typical/Atypical chest pain
MJM
Friday, August 11, 2006
Wardround 11viii6
The two minute tutorials this week were about diabetic retinopathy with Clinical features by NM and Management by VJ. Both were well prepared talks for such a broad subject. Dr Mohan gets this week’s prize (quoted his sources which included this which is worth a look. He has also posted more information at http://kmneo.blogspot.com/
This week’s reading was "Stepford doctors": an allegory. GM Sayers. Medical Humanities 2006;32:57-58. It seems more an analogy than allegory, and I am not sure that I agree completely with the article. Presumably it has been written to stimulate thought (and discussion) regarding the part doctors play in health care. It ends with this paragraph: This allegory cannot be concluded because it is ongoing. Some doctors refused to "reform" and transform into "Stepford doctors". They believed that their allegiance lay with their patients and not the masters. Those who did not leave the profession (as many did) remain part of the lineage from which they stemmed. They continue to defend the freedom to practise the sort of medicine their patients want. Only time will tell whether these doctors become extinct or manage to inspire their followers to reclaim their vocation. What do you think?
Next week’s reading is The plague of Athens. The link for reading is in last week’s post (see below). You must decide on a diagnosis and will have two minutes to make your case on the 18th August.
Interesting topics this week
Hyperkalaemia (beware Lo-salt preparations)
Septic shock
Atrial fibrillation
Toxic confusional states
Cannabis lung
MJM
Sunday, August 06, 2006
Wardround 4viii6
This week’s two minute tutorials were about electrolytes:
Sodium Dr Mohan (excellent handout)
Creatinine Dr Joshi
Glucose
Calcium Dr Sykes
Magnesium MJM
This week’s prize goes to Dr Sykes. Would each of you post a sentence in the comments section about your subject please.
Next week's assignments are:
Clinical features of diabetic retinopathy (Dr Mohan)
Management of retinopathy (Dr Joshi)
Non-retinopathic eye disease in diabetes (up for grabs)
Two minutes please, keep it concise and precise and quote your sources.
The reading for this week was: Reassurance and the Warning on the Label. Jerome Lowenstein, from The Midnight Meal and other essays about Doctors, Patients, and Medicine (1997). In the essay Dr Lowenstein highlights the difference between advice and reassurance. We often attach warnings to advice given to patients along the lines of ..."we cannot predict whether it will work" or "we do not know what the effects will be". But reassurance must be free of such caveats since it is undermined by such additions. Do you agree?
The reading for Friday 11th will be "Stepford doctors": an allegory. GM Sayers. Medical Humanities 2006;32:57-58. Read and think.
The reading for Friday 18th is a description of the plague of Athens, written in 431BC by Thucydides in The History of the Peloponnesian War. If you click on the link it will take you to a copy of the piece. The web page begins with chapter VI, but you can skip down to chapter VII (unless you would like to read about the war). If you cannot find the right section, press ctrl-F and type in plague. The challenge is to make a diagnosis. You will have two minutes to make your case for the diagnosis of your choice. This will be in place of the usual two minute tutorials that week.
Interesting topics this week:
Hyponatraemia
MJM
Sodium Dr Mohan (excellent handout)
Creatinine Dr Joshi
Glucose
Calcium Dr Sykes
Magnesium MJM
This week’s prize goes to Dr Sykes. Would each of you post a sentence in the comments section about your subject please.
Next week's assignments are:
Clinical features of diabetic retinopathy (Dr Mohan)
Management of retinopathy (Dr Joshi)
Non-retinopathic eye disease in diabetes (up for grabs)
Two minutes please, keep it concise and precise and quote your sources.
The reading for this week was: Reassurance and the Warning on the Label. Jerome Lowenstein, from The Midnight Meal and other essays about Doctors, Patients, and Medicine (1997). In the essay Dr Lowenstein highlights the difference between advice and reassurance. We often attach warnings to advice given to patients along the lines of ..."we cannot predict whether it will work" or "we do not know what the effects will be". But reassurance must be free of such caveats since it is undermined by such additions. Do you agree?
The reading for Friday 11th will be "Stepford doctors": an allegory. GM Sayers. Medical Humanities 2006;32:57-58. Read and think.
The reading for Friday 18th is a description of the plague of Athens, written in 431BC by Thucydides in The History of the Peloponnesian War. If you click on the link it will take you to a copy of the piece. The web page begins with chapter VI, but you can skip down to chapter VII (unless you would like to read about the war). If you cannot find the right section, press ctrl-F and type in plague. The challenge is to make a diagnosis. You will have two minutes to make your case for the diagnosis of your choice. This will be in place of the usual two minute tutorials that week.
Interesting topics this week:
Hyponatraemia
MJM
Tuesday, August 01, 2006
Wardround 1viii6

A warm welcome to the new clutch. I am afraid that this weblog will be the source of much work for you. Check it each week to confirm your assignments for the two minute tutorials and the paper for ‘reading and thinking’.
Since you will be finding your feet for the first few days, there will be only very simple two minute tutorials, but I will allocate them personally.
The reading for this week is: Reassurance and the Warning on the Label. Jerome Lowenstein, from The Midnight Meal and other essays about Doctors, Patients, and Medicine (1997). Read it, think about it, and we can discuss it over coffee on Friday.
Interesting cases this week:
Sick sinus syndrome.
Obstructive uropathy.
MJM
Saturday, July 08, 2006
Wardround 7vii6
A very brief blog this time I'm afraid...must dash to holidays. I have forgotten to bring my notebook (paper not CPU) home, so I will not give comments about this week's talks other than to say that Hannah Gunn's mock GP letter, to illustrate which information we need to pass to GPs, was a stroke of genius. We must make such things a regular feature.
Next week's tutorials are themed about parasites...you know your assignments.
The reading for next week is to be found here and continues the theme of sharing medical information.
There will be a break in the blog for two weeks. MJM
Next week's tutorials are themed about parasites...you know your assignments.
The reading for next week is to be found here and continues the theme of sharing medical information.
There will be a break in the blog for two weeks. MJM
Sunday, July 02, 2006
Wardround 1vii6
It seems a while since the last wardround blog. But it all starts again. This weeks tutorials were about anaemia: Microcytic (EB), Macrocytic (VA), Normocytic (MC), Haemolytic (HG), Investigation (RS), Marrow failure (GT). I find that I gave equal marks to all so the winner of best talk will have to be based on gestalt. Prize therefore to Dr Chee for clarity and making it concise.
Next week's theme is Polymyalgia Rheumatica: assignments as listed below. Keep to two minutes and don't put in too much. I am going to add another limit...no more than 50 words on your handout.
Polymyalgia Rheumatica (and GCA if you like):
What the patient needs to know (house officer)
What the GP needs to know (HG)
Diagnosis (EB)
Treatment (RS)
Clinical Epidemiology (MC)
Prognosis (GT)
Next week's paper for discussion: Doctors’ use of euphemisms and their impact on patients’ beliefs about health: an experimental study of heart failure. Taylor M, Ogden J. Patient Education and Counseling. Volume 57, Issue 3 , June 2005, Pages 321-326. http://dx.doi.org/10.1016/j.pec.2004.09.001
MJM
Next week's theme is Polymyalgia Rheumatica: assignments as listed below. Keep to two minutes and don't put in too much. I am going to add another limit...no more than 50 words on your handout.
Polymyalgia Rheumatica (and GCA if you like):
What the patient needs to know (house officer)
What the GP needs to know (HG)
Diagnosis (EB)
Treatment (RS)
Clinical Epidemiology (MC)
Prognosis (GT)
Next week's paper for discussion: Doctors’ use of euphemisms and their impact on patients’ beliefs about health: an experimental study of heart failure. Taylor M, Ogden J. Patient Education and Counseling. Volume 57, Issue 3 , June 2005, Pages 321-326. http://dx.doi.org/10.1016/j.pec.2004.09.001
MJM
Friday, June 23, 2006
EULAR 2006

EULAR 2006 Odds and ends (posters):
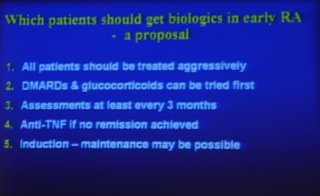
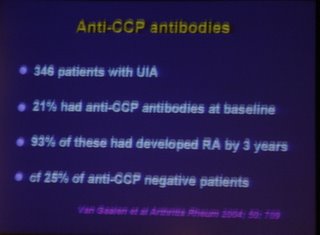
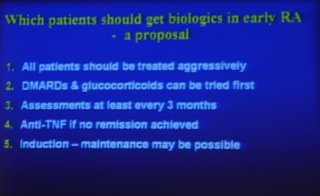
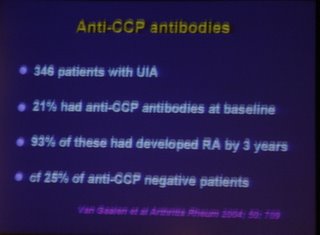
ESPOIR cohort: predicting the evolution of undifferentiated Inflammatory arthritis into RA. Multiple regression analysis gave the following odds ratios: Symmetrical onset 2.5; morning stiffness >60 minutes 1.7; synovitis >6 4.1; RF+ 2.2; anti-CCP+ 5.6. (Abstract THU0103). This does highlight the importance of anti-CCP. I hope we can get it soon.
Use of MTX (10-20mg/week) in Chronic pyrophosphate arthropathy. Tiny uncontrolled study of five patients but all reported as significantly improved. (THU0468)
Use of questionnaires to ask about recent medical and demographic events to improve efficiency in clinics (by T Pincus THU0130). I wonder if we should add something like this to our own clinic questionnaires?
Anti-CCP antibodies may predict which patients with palindromic rheumatism will evolve into RA (FRI0044). But what good that will do remains to be seen.
Patients on adalimumab seem to respond normally to immunisation against pneumococci and influenza (FRI0064). Which is I suppose useful.
Etanercept reported as effective in refractory PMR (series of 3, uncontrolled study) FRI0267. Significant changes in pain scores and HAQ of the order of 50%, but it only seemed to achieve a reduction in prednisolone of 5-7.5mg.
Two case reports of successful treatment of chronic tophaceous gout with infliximab. (FRI0491, FRI0496). Hmmm?
A Dutch study showed acute gout was more common in the Spring (FRI0495). I will mull over how that will change my practice.
A survey of UK rheumatologists (which included me!) showed that the BNF colchicine regime was used by only a minority. More than half used colchicine bd or tds.(FRI0498)
I have put the abstract numbers in, since you can get the abstracts online from the eular website http://www.eular.org
So what questions are raised by this meeting?

1. Can we be any better at predicting which patients with undifferentiated inflammatory arthritis will develop damaging arthritis?
Possibly, we know that anti-CCP positive patients with UIA are more likely to develop RA: 21% of UIA are CCP+, of those 93% develop RA, but 25% of CCP- also develop RA. In one talk this meeting it was suggested that a clinical prediction rule using 9 variables (including CCP) was able to assign patients such that only 6% of those predicted not to develop RA actually did go on to RA. This needs to be tested prospectively but if it does hold true, we need to consider if delaying treatment in this 6% with RA is acceptable. Clearly some members of the audience did not think it was. I will continue to treat all UIA/PISA with DMARDs for the time being.
I do wonder though if it might be feasible to use anti-CCP status to inform decisions about withdrawing DMARDs in that group which enters remission. They have either really gone into remission or are held in remission by treatment. It would seem reasonable to give greater consideration to stopping DMARDs in the CCP negative cases...but I do not think there is evidence to support this.
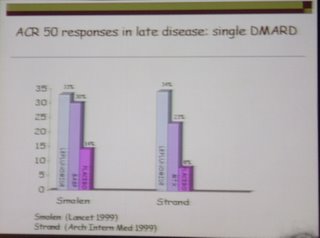
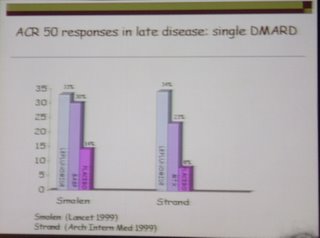
2. Which DMARD to use in early inflammatory arthritis?
The easy answer is...one that works. But which to try first? If monotherapy is used it looks as if it should be with more intensive follow-up and tight control of synovitis (IM/IA steroids?). I tend to use MTX but the TICORA study did well with SASP as the initial drug.
MJM

Thursday, June 22, 2006
EULAR 2006
Today has been a busy day at the conference, and my internet time is running out...so this will have to be quick, key points only.
The question was raised again as to whether Anti-CCP positive/negative Rheumatoid disease is different. One postulation is that proteins become citrillunated (by smoking for example) and subjects with the shared epitope variants of DR4 then develop anti-CCP antibodies. The Prompt study from yesterday showed that MTX had no impact on the evolution of anti-CCP negative undifferentiated arthritis to RA, but in anti-ccp positive UA MTX significantly reduced the evolution to RA. Treatment with anti-BLys antibodies was also less effective in CCP negative RA.
Much talk about the best use of DMARDs...use early in adequate doses (dare I say aggressive doses?), monitor frequently and adjust to control disease (as in the TICORA study). Consider checking anti-CCP status in RF negative inflammatory arthrtis.
Treatment of refractory RA (ie failed MTX and one anti-TNF)
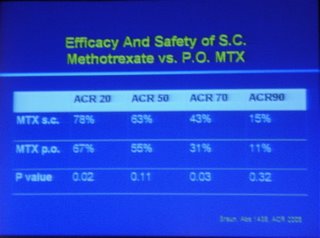
Optimise DMARD: dose to 25mg/week, change PO to SubCut, use a split dose (more on that later)
Optimise Anti-TNF: dose, frequency
Switch TNF: more useful for secondary failures (ie worked initially) than primary failures
Use another biologic: Abatacept, Rituximab.
Just a short note for now since my internet connection is about to run out of money.
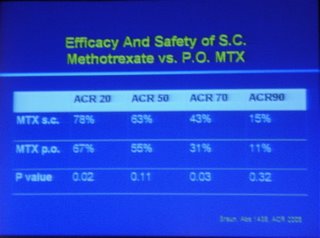



PS split dose MTX: taking some in the evening and some next morning may improve bioavailability of higher doses (above 15mg) but the evidence is limited. Worth a try if all else fails though.
MJM
The question was raised again as to whether Anti-CCP positive/negative Rheumatoid disease is different. One postulation is that proteins become citrillunated (by smoking for example) and subjects with the shared epitope variants of DR4 then develop anti-CCP antibodies. The Prompt study from yesterday showed that MTX had no impact on the evolution of anti-CCP negative undifferentiated arthritis to RA, but in anti-ccp positive UA MTX significantly reduced the evolution to RA. Treatment with anti-BLys antibodies was also less effective in CCP negative RA.
Much talk about the best use of DMARDs...use early in adequate doses (dare I say aggressive doses?), monitor frequently and adjust to control disease (as in the TICORA study). Consider checking anti-CCP status in RF negative inflammatory arthrtis.
Treatment of refractory RA (ie failed MTX and one anti-TNF)
Optimise DMARD: dose to 25mg/week, change PO to SubCut, use a split dose (more on that later)
Optimise Anti-TNF: dose, frequency
Switch TNF: more useful for secondary failures (ie worked initially) than primary failures
Use another biologic: Abatacept, Rituximab.
Just a short note for now since my internet connection is about to run out of money.



PS split dose MTX: taking some in the evening and some next morning may improve bioavailability of higher doses (above 15mg) but the evidence is limited. Worth a try if all else fails though.
MJM
Sunday, June 04, 2006
History of Thiamine
Wardround 2vi6
This week’s two minute tutorials were themed around diabetes:
Diagnosis and investigation (JCM)
Presentations (CC)
Complications (EB)
Oral hypoglycaemics (JA)
Diet (RS)
Insulin ℞ (VA)
Well researched talks overall, and several well timed to the two minutes. I was surprised by the fact that by 55 years of age 35% of patients with T1DM would have died from MI. Nice touch by VA to have used the diabetes specialist nurses as a source. If you want to read a quick (<15 minutes ) review of DM try these documents:
http://www.emedicine.com/emerg/topic133.htm
http://www.emedicine.com/emerg/topic134.htm
For next week the topic is renal:
Assessment of renal function (JCM)
Causes of acute renal failure (VA)
Management of ARF other than dialysis (EB)
Dialysis in ARF (CC)
Complications of CRF (PS)
Remember, two minutes only, so keep it concise and precise. Quote your sources.
The reading last week was A Mysterious Death. Oldach DW et al. NEJM 1998; 338(24):1763-1769. This is a case discussion of the death of Alexander the Great. The systematic approach to differential diagnosis is instructive, and the paper should act as a trigger to revise the features of those diseases mentioned. Perhaps if we do this paper again it would be useful to combine it with the two minute talks to revise the features of the major diagnoses discussed? Comments please?
For next time the reading is: Spellbinding and spellbreaking in convalescence. George Day. Lancet 1961; 279 (7222):211-213. Log on to the NHS Scotland elibrary with your Athens password and choose the Lancet. You will be offered several sources, choose the Sciencedirect Lancet site. If you have trouble (you shouldn’t) come and find me...I have a hard copy.
MJM
Diagnosis and investigation (JCM)
Presentations (CC)
Complications (EB)
Oral hypoglycaemics (JA)
Diet (RS)
Insulin ℞ (VA)
Well researched talks overall, and several well timed to the two minutes. I was surprised by the fact that by 55 years of age 35% of patients with T1DM would have died from MI. Nice touch by VA to have used the diabetes specialist nurses as a source. If you want to read a quick (<15 minutes ) review of DM try these documents:
http://www.emedicine.com/emerg/topic133.htm
http://www.emedicine.com/emerg/topic134.htm
For next week the topic is renal:
Assessment of renal function (JCM)
Causes of acute renal failure (VA)
Management of ARF other than dialysis (EB)
Dialysis in ARF (CC)
Complications of CRF (PS)
Remember, two minutes only, so keep it concise and precise. Quote your sources.
The reading last week was A Mysterious Death. Oldach DW et al. NEJM 1998; 338(24):1763-1769. This is a case discussion of the death of Alexander the Great. The systematic approach to differential diagnosis is instructive, and the paper should act as a trigger to revise the features of those diseases mentioned. Perhaps if we do this paper again it would be useful to combine it with the two minute talks to revise the features of the major diagnoses discussed? Comments please?
For next time the reading is: Spellbinding and spellbreaking in convalescence. George Day. Lancet 1961; 279 (7222):211-213. Log on to the NHS Scotland elibrary with your Athens password and choose the Lancet. You will be offered several sources, choose the Sciencedirect Lancet site. If you have trouble (you shouldn’t) come and find me...I have a hard copy.
MJM
Monday, May 22, 2006
Wardround 19v6
 A thing of beauty is a joy forever. Even my nemesis pictured here.
A thing of beauty is a joy forever. Even my nemesis pictured here.This week's two minute tutorials were a challenge; such broad subjects, inflammatory bowel disorders, so little time. Very interesting though. If you email your talks to me I will incorporate them in the blog.
The week's Reading had been The Iowa Car Crop by S E Landsberg. I had asked you why you thought I had chosen it and how it might be relevent to medicine. HmmmH.... I admit to being seduced by the first three lines: "A thing of beauty is a joy forever and there is nothing more beautiful than a succinct and flawless argument." The paper was chosen because any critical criteria I may use for choosing our reading were corrupted by the paper's rhetoric (or more correctly the author's rhetoric). The opening lines appealed to me and so the paper was chosen. The relevance to medicine is two fold. Firstly beware accepting or rejecting papers because of rhetoric rather than substance. the second part relates to the ships that disappear over the horizon and return later loaded with Toyotas. The author suggests that for an economist to analyse this phenomenon it is not necessary to understand the nature of Japan...it is adequate to imagine it a amagic box which convertts wheat into Toyotas. Diagnoses are similar. It is not always necessary to know everything about a patient's disease (indeed we never know everything) in order to produce a workable management plan. It is only important to know those things which are necessary to produce the plan. I do not know the cause of polymyalgia rheumatica, but I do know the prognosis, complications, treatment and differential diagnosis.
Next week's two minute tutorials are related to Hypertension:
Ace inhibitors (TS)
Beta-blockers (EB)
Calcium channel blockers (AJ)
Diuretics (CC)
Non-drug treatment (JCM)
Investigation of HT (MC)
Keep up the excellent standard. Quote your sources, keep it concise and precise.
The reading for the week is A mysterious death. David W Oldach, Robert E Richard, Eugene N Borza, R Michael Benitez. The New England Journal of Medicine. Jun 11, 1998.Vol.338, Iss. 24; pg. 1764, 6 pgs
I am away this week, see you next week. MJM
Sunday, May 14, 2006
Saturday, May 13, 2006
Wardround 12v6
 This week’s theme was Spirochaetal diseases, Syphilis, Yaws, Pinta, Leptospirosis and Lyme disease. I think this was quite a challenge, but the talks were excellent and a good stimulus for further reading on my part. I will try to get the fact sheets you made scanned and made available, but if you could email the files to me it would be easier.
This week’s theme was Spirochaetal diseases, Syphilis, Yaws, Pinta, Leptospirosis and Lyme disease. I think this was quite a challenge, but the talks were excellent and a good stimulus for further reading on my part. I will try to get the fact sheets you made scanned and made available, but if you could email the files to me it would be easier.Next week’s theme is inflammatory bowel diseases: UC, Crohn’s, Coeliac, C.difficile. You have your assignments. Two minute talks please, concise and precise.
This week’s reading was Clinical craft: a lesson from Liverpool. D M Gore Journal of Medical Ethics 27:74-75 (2001). "Surely now is a good time to revisit the concept of clinical craft. ... we also need a certain amount of pride to keep up our morale. By celebrating our craft we can identify with skilled workers anywhere." Pride in a job well done is a precious crop, full of nourisment for the spirit and vitamins for the soul. It is all too easy to tend the plant but allow the fruit to wither on the branch or fall to rot on the ground. My advice: Take some time each week to reflect on what you have achieved as an individual or as part of a team.
For next week I have chosen a different subject: The Iowa Car Crop, S E Landsburg, from The Armchair Economist (1995). I have left a copy on the ward. I would like you to read this and ponder two things: why I have chosen it and what relevance it has for medicine.
Interesting topics this week
SIRS (Systemic inflammatory response syndrome) with hypoxia, eosinophilia, myalgia and anti-MPO antibodies.
CSS
SIRS
Eosinophilia myalgia syndrome (as a fascinoma)
Ultrasound for pleural effusions
Staph. septicaemia. How to confirm SBE; do you know the Duke criteria? And if you do....Are they useful in clinical practice?
MJM
Sunday, May 07, 2006
Wardround 5v6
The two minute tutorials this week were themed around common drugs: Furosemide, Coamoxiclav, Metformin, Citalopram, Omeprazole. It is always useful to focus on those things that would otherwise be part of the background. It was clear that there were important actions one can take when assessing a patient taking one of these agents.
Has it been effective? Is it still needed? Can it be withdrawn? should that be rapid or slow? Are there warnings for the patient? do those warnings change the patient's views about using the treatment.
What sticks in my mind? Do not stop citalopram abruptly, warn patients on PPIs about infection risks (and how to reduce them), warn patients to stop metformin if they become breathless or are vomiting, beware clavulanic acid (coamoxiclav) with liver disease.
The reading this week was Bandolier: What patients think. A comment on the Original paper: PN Trewby et al. Are preventative drugs preventive enough? A study of patients' expectation of benefits from preventive drugs. Clinical Medicine 2002 2: 527-533. There seems to be a gap between the risk/benefit thresholds exhibited by doctors and patients, at least in so far as this study shows.
The Bandolier comment includes "This is an interesting and imaginative paper that tells us what patients think. Half were happy to take a preventive drug if the hypothetical five year absolute risk reduction was 20%, or an NNT of 5. ..... There is a clear discrepancy. Few preventive medicines for preventing heart attacks would seem to meet patient expectation.... the power of the doctor to advise. If their doctor recommended it, more than twice as many subjects would take the medicine. This, though, imposes a significant burden on doctors properly to inform their patients. Much less attention has been paid to how patients think about their own versus population benefit, and especially how the information is presented. "
Interesting topics this week:
Trigeminal neuralgia and Lyme disease
Next week's two minute talks are themed around spirochaetes (I hope Dr Jones has handed out the assignments).
The reading for next week is: Clinical craft: a lesson from Liverpool. D M Gore Journal of Medical Ethics 27:74-75 (2001)
MJM
Has it been effective? Is it still needed? Can it be withdrawn? should that be rapid or slow? Are there warnings for the patient? do those warnings change the patient's views about using the treatment.
What sticks in my mind? Do not stop citalopram abruptly, warn patients on PPIs about infection risks (and how to reduce them), warn patients to stop metformin if they become breathless or are vomiting, beware clavulanic acid (coamoxiclav) with liver disease.
The reading this week was Bandolier: What patients think. A comment on the Original paper: PN Trewby et al. Are preventative drugs preventive enough? A study of patients' expectation of benefits from preventive drugs. Clinical Medicine 2002 2: 527-533. There seems to be a gap between the risk/benefit thresholds exhibited by doctors and patients, at least in so far as this study shows.
The Bandolier comment includes "This is an interesting and imaginative paper that tells us what patients think. Half were happy to take a preventive drug if the hypothetical five year absolute risk reduction was 20%, or an NNT of 5. ..... There is a clear discrepancy. Few preventive medicines for preventing heart attacks would seem to meet patient expectation.... the power of the doctor to advise. If their doctor recommended it, more than twice as many subjects would take the medicine. This, though, imposes a significant burden on doctors properly to inform their patients. Much less attention has been paid to how patients think about their own versus population benefit, and especially how the information is presented. "
Interesting topics this week:
Trigeminal neuralgia and Lyme disease
Next week's two minute talks are themed around spirochaetes (I hope Dr Jones has handed out the assignments).
The reading for next week is: Clinical craft: a lesson from Liverpool. D M Gore Journal of Medical Ethics 27:74-75 (2001)
MJM
Tuesday, May 02, 2006
Common drugs
This week’s paper for discussion is not a real paper, but a comment. I did promise a brief paper for this week. You can of course read the original if it suits you to so do. The reading is from Bandolier: What patients think.
Original paper: PN Trewby et al. Are preventative drugs preventive enough? A study of patients' expectation of benefits from preventive drugs. Clinical Medicine 2002 2: 527-533.
The two minute tutorials are themed about common drugs: Furosemide, Metformin, Citalopram, Omeprazole, Coamoxiclav. Remember, two minutes only. Be concise and precise, quote sources and a handout please.
MJM
Original paper: PN Trewby et al. Are preventative drugs preventive enough? A study of patients' expectation of benefits from preventive drugs. Clinical Medicine 2002 2: 527-533.
The two minute tutorials are themed about common drugs: Furosemide, Metformin, Citalopram, Omeprazole, Coamoxiclav. Remember, two minutes only. Be concise and precise, quote sources and a handout please.
MJM
Sunday, April 16, 2006
Saturday, April 15, 2006
Wardround 14iv6
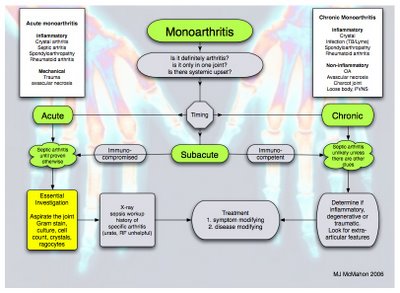
This week’s two minute tutorial theme was monoarthritis. We heard about Gout (CC), Investigation (GYD), septic arthritis (KP), RA (DK), epidemiology (MH) and pseudogout (SM).
I found the talks detailed and well delivered. A deal of work obviously went into each talk but I award the prize this week to Dr Pearson for a well presented talk with just the right amount of information for two minutes, a clear handhout and citing of sources.
In the approach to monoarthritis the important considerations are:
Is this a problem in a joint (arthritis)?
Is it monoarthritis (or are more joints involved)?
Then get some synovial fluid or get someone who can and ask yourself "How likely is sepsis? can I exclude it?"
The latter question is critical especially in the setting of acute monoarthritis, or sub-acute monoarthritis in the immunocompromised patient. I generally take the view that when I cannot show it is not sepsis, it should be treated as septic arthritis until an alternative diagnosis is found.
Remember that gonococcal arthritis presents differently to non-gonococcal pyogenic arthritis. (have a look at UpToDate)
A podcast will follow soon, until then, a useful description can be found in Infection and arthritis.
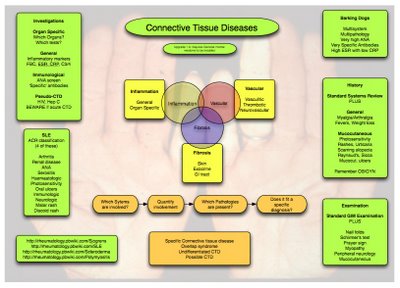
Next week’s theme is connective tissue diseases:
SLE (GYD)
Sjögren’s Syndrome (PK)
Myositis (MH)
Systemic sclerosis (CC)
Behçet’s disease (SM)
Diagnosis (DK)
These will be difficult to squeeze into two minutes, so you will have to choose your information carefully. Try to think about the assignment as relating to a patient coming to the clinic. What are the important points you would highlight for a student? Be concise and precise, and cite your sources. And why not try to learn a little more be asking yourself what you know about the subjects your colleagues will be talking about?
Interesting topics this week:
I recommend you have a look at the NEJM’s video on arterial line placement.
Lobar Collapse
The lobar collapse tutorial.
Migratory arthritis (turned out to be CPPD, but make sure you know how to investigate Rheumatic fever)
Next week’s reading will be The rest is silence. Michael Rowe. Health Affairs, July/August 2002; 21(4): 232-236. I recommend you read this unhurriedly and with plenty of time for reflection.
MJM
I found the talks detailed and well delivered. A deal of work obviously went into each talk but I award the prize this week to Dr Pearson for a well presented talk with just the right amount of information for two minutes, a clear handhout and citing of sources.
In the approach to monoarthritis the important considerations are:
Is this a problem in a joint (arthritis)?
Is it monoarthritis (or are more joints involved)?
Then get some synovial fluid or get someone who can and ask yourself "How likely is sepsis? can I exclude it?"
The latter question is critical especially in the setting of acute monoarthritis, or sub-acute monoarthritis in the immunocompromised patient. I generally take the view that when I cannot show it is not sepsis, it should be treated as septic arthritis until an alternative diagnosis is found.
Remember that gonococcal arthritis presents differently to non-gonococcal pyogenic arthritis. (have a look at UpToDate)
A podcast will follow soon, until then, a useful description can be found in Infection and arthritis.
Next week’s theme is connective tissue diseases:
SLE (GYD)
Sjögren’s Syndrome (PK)
Myositis (MH)
Systemic sclerosis (CC)
Behçet’s disease (SM)
Diagnosis (DK)
These will be difficult to squeeze into two minutes, so you will have to choose your information carefully. Try to think about the assignment as relating to a patient coming to the clinic. What are the important points you would highlight for a student? Be concise and precise, and cite your sources. And why not try to learn a little more be asking yourself what you know about the subjects your colleagues will be talking about?
Interesting topics this week:
I recommend you have a look at the NEJM’s video on arterial line placement.
Lobar Collapse
The lobar collapse tutorial.
Migratory arthritis (turned out to be CPPD, but make sure you know how to investigate Rheumatic fever)
Next week’s reading will be The rest is silence. Michael Rowe. Health Affairs, July/August 2002; 21(4): 232-236. I recommend you read this unhurriedly and with plenty of time for reflection.
MJM
Monday, March 27, 2006
Wardround 24iii6
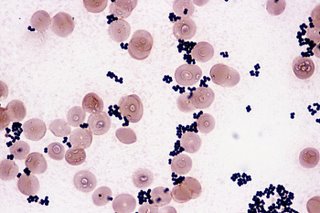
The two minute tutorials this week were themed around fungal infection. Amphotericin B (PS); New antifungals (GYD); Aspergillus (HG) *; Candida in catheters (KP); Cryptococcus (DK). The general quality of presentation was excellent this week and I was pleased to see the re-emergence of visual aids and citing of sources. Prize this week to Dr Gunn.
I found doctorfungus.org an interesting source for revision.
Next week we will stick with infectious disease but viruses this time. The assignments are related to Hepatitis B:
Treatment of chronic Hep B (DK)
Prevention/immunisation (KP)
Interpretation of serology (HG)
Clinical epidemiology (GYD)
Acute fulminant hepatitis (PS)
Be precise and concise, just two minutes. Cite your sources and let’s have visual aids.
This week’s reading had been Laments, and I would like to continue the discussion with Jerome Lowenstein’s essay “Can you teach compassion”. I presume he meant “Can one teach compassion” but, you never know, he may have meant it to be personal. It is not available on the internet but my copy will be available on the ward.
Rather a short post this week as my weekend has been spent away from internet access.
MJM
I found doctorfungus.org an interesting source for revision.
Next week we will stick with infectious disease but viruses this time. The assignments are related to Hepatitis B:
Treatment of chronic Hep B (DK)
Prevention/immunisation (KP)
Interpretation of serology (HG)
Clinical epidemiology (GYD)
Acute fulminant hepatitis (PS)
Be precise and concise, just two minutes. Cite your sources and let’s have visual aids.
This week’s reading had been Laments, and I would like to continue the discussion with Jerome Lowenstein’s essay “Can you teach compassion”. I presume he meant “Can one teach compassion” but, you never know, he may have meant it to be personal. It is not available on the internet but my copy will be available on the ward.
Rather a short post this week as my weekend has been spent away from internet access.
MJM
Saturday, March 18, 2006
Neuropathy
MP3 File
Recommended reading: Clinical Evaluation and Investigation of neuropathy. Hugh J Willison and John B Winer. Journal of Neurology Neurosurgery and Psychiatry 2003;74:ii3
Friday, March 17, 2006
Wardround 17iii6

This week’s two minute tutorials were themed around transfusion (blood, platelets, FFP, cryoprecipitate, immunoglobulins and albumin). I was pleased to see that handouts have made a come back, but our original idea had been that visual aids would be brief revision notes rather than detailed notes. Have a look at mediglyphics.
The British Committee for Standards in Haematology (BCSH) have a collection of guidelines on transfusion that are well worth browsing.
The week’s reading had been Doctors and thin slicing. Interesting findings which none of the senior colleagues who read it found surprising. Certainly food for thought. I attended a course about communication last year and was told that communication was more important than what a doctor actually did with a patient. This strikes me as being unlikely. Worse though, if accepted as a correct premise it could undermine the practice of medicine. Is satisfaction a reasonable outcome measure when used alone? Is satisfaction now the same as satisfaction later? Richard Wakeford wrote a letter to the BMJ in 2003 (BMJ 2003;327:161 (19 July), doi:10.1136/bmj.327.7407.161) I quote a section of it here...
In its revalidation guidance documents for doctors the GMC says that one good professional comparison is with airline pilots. This comparison is helpful. Imagine two airlines, whose pilots' revalidation arrangements are on the following bases:
• Airline A—flight simulator skills tests, including rarely met but crucial challenges; a thorough medical examination
• Airline B—informal personal development plans, agreed privately with a colleague, maybe of their choice; cabin crew and passenger surveys of the gentleness of their landings and the clarity of their communications; a self declaration of sobriety, health, and honesty.
For the sake of argument, let us assume that one in every 15 pilots is shown by research to have at some point in their career an alcohol or other substance abuse problem. Which airline would you travel with?
Interesting topics this week
Tophaceous gout, which reminds me of this interesting paper regarding communication of information about gout treatment. Effective management of gout: an analogy. Wortmann R
Am J Med. 1998 Dec;105(6):513-4.
Chronic Q fever
The undiagnosable case (there is no such thing!....I’ll do a podcast on this sometime). We have certainly had some diagnostic challenges lately.
Next week’s reading for discussion continues the communication theme, The patient’s lament: hidden key to effective communication: how to recognise and transform. B Bub. Medical humanities 2004;30:63-69
The two minute tutorial topic for next week is Fungi. I will give more info on specific assignments when ID doc espeaks to me.
The team bids goodbye to Dr CT this week. No more dayglo stethoscopes.
MJM
Friday, March 10, 2006
Wardround 10iii6
The theme this week was everyday microbes with two minute talks on: S. aureus, Str. pneumoniae, E. coli, and P. aeruginosa. I was pleased that so much information was gathered, and if you would like to read a little more have a look at Medical Microbiology for some further basic information. If you would like a little more information on the military use of Serratia marcescans in San Francisco, have a look at the wikipedia entry.
Next week’s theme is blood transfusion products.
Blood
FFP & Cryo
Platelets
IVIg
Just to repeat the rules: two minutes on the subject, which should be a talk rather than a reading. Quote your sources and use handouts to illustrate points.
The reading for next week is Doctors and Thin Slicing from Blink, by Malcolm Gladwell.
Interesting cases this week
Myocardial infarction and diabetes
....and more at xxxxxxx
Trifascicular block
Bronchiolitis and macrolides
Mycobacterium avium complex
Cricoarytenoid arthritis (a patient with rheumatoid who could no longer play the trumpet!)
MJM
Next week’s theme is blood transfusion products.
Blood
FFP & Cryo
Platelets
IVIg
Just to repeat the rules: two minutes on the subject, which should be a talk rather than a reading. Quote your sources and use handouts to illustrate points.
The reading for next week is Doctors and Thin Slicing from Blink, by Malcolm Gladwell.
Interesting cases this week
Myocardial infarction and diabetes
....and more at xxxxxxx
Trifascicular block
Bronchiolitis and macrolides
Mycobacterium avium complex
Cricoarytenoid arthritis (a patient with rheumatoid who could no longer play the trumpet!)
MJM
Sunday, March 05, 2006
Friday, March 03, 2006
Wardround 3iii6
The two minute tutorials this week were about aortic stenosis. Epidemiology (CT), clinical features (BK), investigation (HG), and treatment (CC). There are plenty of brief summaries on the net but this is a subject worthy of more detailed understanding and knowledge for GIM trainees. Certainly the investigation, assessment and indications for surgery should roll off your tongue with ease. The prize for this week’s talk goes to Dr Tuck, for a concise summary with sources quoted. It is about time someone stepped up to the mark and knocked her off the top spot.
The discussion paper this week was The Company We Keep: Why Physicians Should Refuse to See Pharmaceutical Representatives. Howard Brody, Annals of Family Medicine 2005;3:82-85. I particularly like the ‘fanciful analogy’ in the paper’s introduction: read it for yourself. I will leave you to muse over one of the conclusions. Reps are not evil, but they are time-consuming and serve interests that often are at odds with those of our patients. To spend time with reps in a manner that preserves professional integrity would require both refusing to accept their gifts and spending a great deal of valuable time double-checking their information. I propose that the vast majority of physicians could spend their time in better ways. Do you feel this is true? Will you be putting your time to better use?
Next week’s reading continues the ethics theme and though the paper relates to research, you should decide if the ideas give any insights into medical practice. Can Mary Shelley’s Frankenstein be read as an early research ethics text? H Davies, Medical Humanities Jun 01, 2004 30: 32-35.
Next week’s theme is basic microbiology. Two minutes please on the following:
Staphylococcus aureus (CC)
Streptococcus pneumoniae (BK)
Escherichia coli (HG)
Pseudomonas aeruginosa (CT)
Interesting topics this week
Ecthyma Gangrenosum
Coma, look at the coma section of www.eboncall.org
Agranulocytosis
And review your knowledge of the normal ECG
MJM
The discussion paper this week was The Company We Keep: Why Physicians Should Refuse to See Pharmaceutical Representatives. Howard Brody, Annals of Family Medicine 2005;3:82-85. I particularly like the ‘fanciful analogy’ in the paper’s introduction: read it for yourself. I will leave you to muse over one of the conclusions. Reps are not evil, but they are time-consuming and serve interests that often are at odds with those of our patients. To spend time with reps in a manner that preserves professional integrity would require both refusing to accept their gifts and spending a great deal of valuable time double-checking their information. I propose that the vast majority of physicians could spend their time in better ways. Do you feel this is true? Will you be putting your time to better use?
Next week’s reading continues the ethics theme and though the paper relates to research, you should decide if the ideas give any insights into medical practice. Can Mary Shelley’s Frankenstein be read as an early research ethics text? H Davies, Medical Humanities Jun 01, 2004 30: 32-35.
Next week’s theme is basic microbiology. Two minutes please on the following:
Staphylococcus aureus (CC)
Streptococcus pneumoniae (BK)
Escherichia coli (HG)
Pseudomonas aeruginosa (CT)
Interesting topics this week
Ecthyma Gangrenosum
Coma, look at the coma section of www.eboncall.org
Agranulocytosis
And review your knowledge of the normal ECG
MJM
Monday, February 27, 2006
Sunday, February 19, 2006
Saturday, February 18, 2006
Wardround 17ii6
This week’s reading and two minute tutorials were themed around epilepsy. The turn out was a little poor with only MJM (epidemiology), CC (investigations) and HG (classification) stepping up to face the music. So perhaps we can repeat this subject in a few weeks. I recommend the SIGN national clinical guideline No.70, Diagnosis and Management of epilepsy in Adults (from April 2003, updated 2005). The Quick guide is well worth a look for revision.
The reading for the week was The Falling Sickness, Jones J, Southern Medical Journal 2000;93(12):1169-1172, which I hope was enlightening. Though some of the views of epilepsy described may seem strange, if not outrageous, you should bear in mind that similar ideas may be held by patients with newly diagnosed epilepsy, or their relatives. It is important to educate patients about the reality of the disease. The aim of treating epilepsy is to render a patient able to live a normal life. Seizure control is but one aspect of this aim.
Next week’s theme is aortic stenosis:
Epidemiology (CT)
Clinical effects (BK)
Investigations (HG)
Treatment (CC)
Two minutes please, with sources quoted.
The reading for next week is The Company We Keep: Why Physicians Should Refuse to See Pharmaceutical Representatives. Howard Brody. Annals of Family Medicine 2005; 3:82-85.
Interesting cases this week:
Pulmonary eosinophilia
SIADH
Paroxysmal AF
Gout
I will be away next Friday so there will be no blog for 24ii6. I will leave it to Dr Jones to set the assignments. (How about fungal infections?).
MJM
The reading for the week was The Falling Sickness, Jones J, Southern Medical Journal 2000;93(12):1169-1172, which I hope was enlightening. Though some of the views of epilepsy described may seem strange, if not outrageous, you should bear in mind that similar ideas may be held by patients with newly diagnosed epilepsy, or their relatives. It is important to educate patients about the reality of the disease. The aim of treating epilepsy is to render a patient able to live a normal life. Seizure control is but one aspect of this aim.
Next week’s theme is aortic stenosis:
Epidemiology (CT)
Clinical effects (BK)
Investigations (HG)
Treatment (CC)
Two minutes please, with sources quoted.
The reading for next week is The Company We Keep: Why Physicians Should Refuse to See Pharmaceutical Representatives. Howard Brody. Annals of Family Medicine 2005; 3:82-85.
Interesting cases this week:
Pulmonary eosinophilia
SIADH
Paroxysmal AF
Gout
I will be away next Friday so there will be no blog for 24ii6. I will leave it to Dr Jones to set the assignments. (How about fungal infections?).
MJM
Sunday, February 12, 2006
Wardround 10ii6
The reading for this week was Does This Woman Have Osteoporosis? Green AD et al, JAMA 2004; 292: 2890 - 2900.
The paper reports that “no single maneuver is sufficient to rule in or rule out osteoporosis or spinal fracture without further testing. The following yielded the greatest positive likelihood ratios (LR+): weight less than 51 kg, LR+, 7.3 (95% confidence interval [CI], 5.0–10.8); tooth count less than 20, LR+, 3.4 (95% CI, 1.4–8.0); rib-pelvis distance less than 2 finger breadths, LR+, 3.8 (95% CI, 2.9–5.1); wall-occiput distance greater than 0 cm, LR+, 4.6 (95% CI, 2.9–7.3), and self-reported humped back, LR+, 3.0 (95% CI, 2.2–4.1). Conclusions: In patients who do not meet current bone mineral density screening recommendations, several convenient examination maneuvers, especially low weight, can significantly change the pretest probability of osteoporosis and suggest the need for earlier screening. Wall-occiput distance greater than 0 cm and rib-pelvis distance less than 2 finger breadths suggest the presence of occult spinal fracture.” I chose this paper because it described several clinical signs that are not routine for most of us in internal medicine (but perhaps less strange to rheumatologists).
The two minute tutorial theme was Dementia. My congratulations on the choice of subject. As I read/revised this, it became obvious to me that I have not given enough time to formally reviewing the subject. The talks were all well constructed and revised. Timing generally good. having said all that, my prize for this week goes to Dr Tuck.
Next week’s topic is Epilepsy...you have your assignments (I will include them later, but they are left the list at work).
Epidemiology
Important clinical points in the history
Investigation
Social aspects
Treatment
The reading for next week is The Falling Sickness, Jones J, Southern Medical Journal 2000;93(12):1169-1172. (get it from the elibrary)
You may also wish to look over, Epilepsy: historical overview. WHO factsheet no. 168. February 2001
MJM
The paper reports that “no single maneuver is sufficient to rule in or rule out osteoporosis or spinal fracture without further testing. The following yielded the greatest positive likelihood ratios (LR+): weight less than 51 kg, LR+, 7.3 (95% confidence interval [CI], 5.0–10.8); tooth count less than 20, LR+, 3.4 (95% CI, 1.4–8.0); rib-pelvis distance less than 2 finger breadths, LR+, 3.8 (95% CI, 2.9–5.1); wall-occiput distance greater than 0 cm, LR+, 4.6 (95% CI, 2.9–7.3), and self-reported humped back, LR+, 3.0 (95% CI, 2.2–4.1). Conclusions: In patients who do not meet current bone mineral density screening recommendations, several convenient examination maneuvers, especially low weight, can significantly change the pretest probability of osteoporosis and suggest the need for earlier screening. Wall-occiput distance greater than 0 cm and rib-pelvis distance less than 2 finger breadths suggest the presence of occult spinal fracture.” I chose this paper because it described several clinical signs that are not routine for most of us in internal medicine (but perhaps less strange to rheumatologists).
The two minute tutorial theme was Dementia. My congratulations on the choice of subject. As I read/revised this, it became obvious to me that I have not given enough time to formally reviewing the subject. The talks were all well constructed and revised. Timing generally good. having said all that, my prize for this week goes to Dr Tuck.
Next week’s topic is Epilepsy...you have your assignments (I will include them later, but they are left the list at work).
Epidemiology
Important clinical points in the history
Investigation
Social aspects
Treatment
The reading for next week is The Falling Sickness, Jones J, Southern Medical Journal 2000;93(12):1169-1172. (get it from the elibrary)
You may also wish to look over, Epilepsy: historical overview. WHO factsheet no. 168. February 2001
MJM
Saturday, February 04, 2006
Wardround 3ii6
The reading for this week was Hedgehog zoonoses Riley PL, Chomel BB. Emerg Infect Dis. 2005 Jan. I suggested this as a catalyst to promote thought about zoonoses in general rather than intimating the specific importance of our prickly friends in human disease.
The talks were interesting and certainly stimulated discussion, particularly since we had one of our new microbiologists in attendance. Specifics included in discussion were Leptospirosis (icteric and anicteric), Lyme (remember the different clinical patterns in US and UK disease),
Rabies, and Toxoplasmosis.
Learning points: know the local zoonoses; take a history of animal contacts.
A second question was the definition of zoonosis. The World Health Organization defines a zoonosis as an infection or infectious disease transmissible from vertebrate animals to man. Merriam-Webster's Medical Dictionary suggests it is a disease communicable from animals to humans under natural conditions. I was slightly put out to find that my two volume shorter Oxford English dictionary does not list zoonois though it does list zoonosology as the study of the diseases of animals. I believe that the medical term zoonosis is in fact a contraction of the more precise anthropozoonosis, a zoonosis maintained in nature by animals and transmissible to humans. (The American Heritage Stedman's Medical Dictionary). Pedantry award to MJM. I lay down a challenge. Using this last definition find a non-infective anthropozoonosis.
Interesting cases this week:
Cryptococcal meningitis
I would also recommend the Uptodate article (available on the hospital intranet).
Next week’s reading is:
Does This Woman Have Osteoporosis? Green AD et al, JAMA 2004; 292: 2890 - 2900 (Get it from the elibrary)
The two minute tutorials next week are on Dementia: epidemiology, assessment, investigation and treatment. Talks precise and concise please, with some indication of your sources.
MJM
The talks were interesting and certainly stimulated discussion, particularly since we had one of our new microbiologists in attendance. Specifics included in discussion were Leptospirosis (icteric and anicteric), Lyme (remember the different clinical patterns in US and UK disease),
Rabies, and Toxoplasmosis.
Learning points: know the local zoonoses; take a history of animal contacts.
A second question was the definition of zoonosis. The World Health Organization defines a zoonosis as an infection or infectious disease transmissible from vertebrate animals to man. Merriam-Webster's Medical Dictionary suggests it is a disease communicable from animals to humans under natural conditions. I was slightly put out to find that my two volume shorter Oxford English dictionary does not list zoonois though it does list zoonosology as the study of the diseases of animals. I believe that the medical term zoonosis is in fact a contraction of the more precise anthropozoonosis, a zoonosis maintained in nature by animals and transmissible to humans. (The American Heritage Stedman's Medical Dictionary). Pedantry award to MJM. I lay down a challenge. Using this last definition find a non-infective anthropozoonosis.
Interesting cases this week:
Cryptococcal meningitis
I would also recommend the Uptodate article (available on the hospital intranet).
Next week’s reading is:
Does This Woman Have Osteoporosis? Green AD et al, JAMA 2004; 292: 2890 - 2900 (Get it from the elibrary)
The two minute tutorials next week are on Dementia: epidemiology, assessment, investigation and treatment. Talks precise and concise please, with some indication of your sources.
MJM
Friday, January 27, 2006
Wardround 27i6
This week’s discussion papers were Controversies in stable coronary artery disease, Opie LH, et al. Lancet, 2006;367(9504):69-78 and Clinical decision-making: coping with uncertainty. A F West and R R West. Postgraduate Medical Journal 2002;78:319-32.
The controversies are probably best read direct from the paper rather than regurgitated by me but I would like you to consider the points raised in the second paper. Uncertainty is never far away in medicine. We should recognise when there is uncertainty, name it and help patients navigate a course through it. Here are a couple of sections from the paper.
Improving scientific knowledge is clearly a laudable objective, although it may reduce clinical uncertainty less than expected. Pretending that the clinical predicament can be reduced to a series of certainties by the recruitment of "evidence" will not work and unrealistic expectations of that stratagem may make the situation worse. Some degree of uncertainty was always here to stay and evidence, even of the highest quality, is only evidence. There will always be judgments to be made by responsible, informed, and compassionate people. They may not be able to perform these broader roles, in communication, holding anxieties and managing uncertainty, unless trained for and supported in them.
One therapeutic role of a clinician is containing the anxieties aroused in the context of uncertainty, and this role may be becoming more difficult. Reliance on protocols and fear of reprimand may lead to clinicians, in some areas of medical care, abandoning their patients at a time of need.
The reading for next week is:
Hedgehog Zoonoses. PY Riley, BB Chome. Emerging Infectious disease January 2005 Vol.11, No. 1
Next week’s two minute tutorials are semi-freestyle. Two minutes on anything you like, as long as it falls under the heading zoonosis. Extra kudos points available for the best definition of zoonosis.
Interesting topics this week:
Hypomagnesaemic hypoparathyroidism
http://www.emedicine.com/emerg/topic274.htm
http://jasn.asnjournals.org/cgi/content/full/10/7/1616
Hyponatraemic Encephalopathy
Treatment of Hyponatremic Encephalopathy. Smith et al. JAMA.1999; 282: 2298-2299.
Management of Hyponatremia. Kian Peng Goh. American Family Physician Vol. 69/No. 10 (May 15, 2004)
Drug induced agranulocytosis
http://www.jr2.ox.ac.uk/bandolier/band136/b136-5.html
Pneumocystis
A new name (Pneumocystis jiroveci) for pneumocystis from humans. Stringer JR, Beard CB, Miller RF, Wakefield AE. Emerg Infect Dis [serial online] 2002 Sep [date cited];8.
The basics
Hospital acquired pneumonia
MJM
The controversies are probably best read direct from the paper rather than regurgitated by me but I would like you to consider the points raised in the second paper. Uncertainty is never far away in medicine. We should recognise when there is uncertainty, name it and help patients navigate a course through it. Here are a couple of sections from the paper.
Improving scientific knowledge is clearly a laudable objective, although it may reduce clinical uncertainty less than expected. Pretending that the clinical predicament can be reduced to a series of certainties by the recruitment of "evidence" will not work and unrealistic expectations of that stratagem may make the situation worse. Some degree of uncertainty was always here to stay and evidence, even of the highest quality, is only evidence. There will always be judgments to be made by responsible, informed, and compassionate people. They may not be able to perform these broader roles, in communication, holding anxieties and managing uncertainty, unless trained for and supported in them.
One therapeutic role of a clinician is containing the anxieties aroused in the context of uncertainty, and this role may be becoming more difficult. Reliance on protocols and fear of reprimand may lead to clinicians, in some areas of medical care, abandoning their patients at a time of need.
The reading for next week is:
Hedgehog Zoonoses. PY Riley, BB Chome. Emerging Infectious disease January 2005 Vol.11, No. 1
Next week’s two minute tutorials are semi-freestyle. Two minutes on anything you like, as long as it falls under the heading zoonosis. Extra kudos points available for the best definition of zoonosis.
Interesting topics this week:
Hypomagnesaemic hypoparathyroidism
http://www.emedicine.com/emerg/topic274.htm
http://jasn.asnjournals.org/cgi/content/full/10/7/1616
Hyponatraemic Encephalopathy
Treatment of Hyponatremic Encephalopathy. Smith et al. JAMA.1999; 282: 2298-2299.
Management of Hyponatremia. Kian Peng Goh. American Family Physician Vol. 69/No. 10 (May 15, 2004)
Drug induced agranulocytosis
http://www.jr2.ox.ac.uk/bandolier/band136/b136-5.html
Pneumocystis
A new name (Pneumocystis jiroveci) for pneumocystis from humans. Stringer JR, Beard CB, Miller RF, Wakefield AE. Emerg Infect Dis [serial online] 2002 Sep [date cited];8.
The basics
Hospital acquired pneumonia
MJM
Saturday, January 21, 2006
Wardround 20i6
The two minute tutorials for this week are deferred until next week since we were somewhat short of our intellectual quorum. We can discuss the Lancet cardiology paper (see last week's wardound post) in more detail then, but I would like to add some additional reading:
Clinical decision-making: coping with uncertainty. A F West and R R West. Postgraduate Medical Journal 2002;78:319-32. You can get this from the PMJ online site by typing in the volume and page number, or through the elibrary.
Error: I was mistaken in announcing that the CVP tutorials are this month. They are in February. At least this means my lecture notes are ready well ahead of time.
Interesting topics this week
Melioidosis
PUO
A COUNTERBLASTE TO TOBACCO.
by King James I of England, VI of Scotland.
James I and VI (for DK)
Hulusi Behçet
MJM
Clinical decision-making: coping with uncertainty. A F West and R R West. Postgraduate Medical Journal 2002;78:319-32. You can get this from the PMJ online site by typing in the volume and page number, or through the elibrary.
Error: I was mistaken in announcing that the CVP tutorials are this month. They are in February. At least this means my lecture notes are ready well ahead of time.
Interesting topics this week
Melioidosis
PUO
A COUNTERBLASTE TO TOBACCO.
by King James I of England, VI of Scotland.
James I and VI (for DK)
Hulusi Behçet
MJM
Sunday, January 15, 2006
Vipers and ACE inhibitors

Vipers and ACE inhibitors
MP3 File
From viper's venom to drug design: breakthroughs in bioscience
Angiotensin converting enzyme inhibition: from viper to patient. Komajda M. Heart 2000;84 (supp1):i11-i14
Brazilian arrowhead viper
Friday, January 13, 2006
Wardround 13i6
This week's reading was The midnight meal, Jerome Lowenstein. He sums up with “ The challenge is to identify and preserve, or recapture, the critical components of relationships in medicine – between colleagues and between physicians and patients – that we need to preserve. A good first step would be to devise some new equivalent of the midnight meal.” I agree with him. The question for us is how will we make it happen. More from Dr Lowenstein as the year goes on.
This week’s two minute tutorials were about GI bleeding (non-variceal). What can I say about this? A common problem, with an incidence of 100/100000 in the UK. The mortality is about 10% and has changed little in the last 40 years. This does not necessarily mean we are making no headway in treatment because the epidemiology is changing and the age of bleeders is increasing. The Rockall Score uses age, haemodynamic disturbance, comorbidity, OGD findings and diagnosis to predict mortality. See the link below to evidence based on call to read more about the scores. A simple way to convert the score into a ‘ball-park’ mortality figure is to square the score and add on half the square again. If you have a easier way let me know. This week's prize goes to Dr Kidder (excellent timing).
Resources:
Evidence based on-call
Non-variceal upper gastrointestinal haemorrhage:
Guidelines. British Society of Gastroenterology Endoscopy Committee
Gut 2002;51(Suppl IV):iv1–iv6
The reading for next week, and the theme for tutorials is:
Controversies in stable coronary artery disease, Opie LH, et al. The Lancet, 7 January 2006 Volume 367, Issue 9504, Pages 69-78
The themes for next week’s two minute tutorials are sections from the paper; two minutes please on:
Statins MJM SHO
β blockers GAJ SHO
ACE inhibitors FY1
You are free to choose an alternative topic from the paper, but I ask that topics are not duplicated.
Interesting topics this week:
Claudication presenting as hip pain.
The Illusion of Certainty. [Clinical Problem Solving]. Wolinsky AP. NEJM 1996; 335(1): 46-48 (DK has a copy and it is available from the elibrary)
Snake venom and ACE inhibitors (this appeared, partially formed, from the pit of my memory during the wardround. I will check the details and tell all in the next podcast)
MJM
This week’s two minute tutorials were about GI bleeding (non-variceal). What can I say about this? A common problem, with an incidence of 100/100000 in the UK. The mortality is about 10% and has changed little in the last 40 years. This does not necessarily mean we are making no headway in treatment because the epidemiology is changing and the age of bleeders is increasing. The Rockall Score uses age, haemodynamic disturbance, comorbidity, OGD findings and diagnosis to predict mortality. See the link below to evidence based on call to read more about the scores. A simple way to convert the score into a ‘ball-park’ mortality figure is to square the score and add on half the square again. If you have a easier way let me know. This week's prize goes to Dr Kidder (excellent timing).
Resources:
Evidence based on-call
Non-variceal upper gastrointestinal haemorrhage:
Guidelines. British Society of Gastroenterology Endoscopy Committee
Gut 2002;51(Suppl IV):iv1–iv6
The reading for next week, and the theme for tutorials is:
Controversies in stable coronary artery disease, Opie LH, et al. The Lancet, 7 January 2006 Volume 367, Issue 9504, Pages 69-78
The themes for next week’s two minute tutorials are sections from the paper; two minutes please on:
Statins MJM SHO
β blockers GAJ SHO
ACE inhibitors FY1
You are free to choose an alternative topic from the paper, but I ask that topics are not duplicated.
Interesting topics this week:
Claudication presenting as hip pain.
The Illusion of Certainty. [Clinical Problem Solving]. Wolinsky AP. NEJM 1996; 335(1): 46-48 (DK has a copy and it is available from the elibrary)
Snake venom and ACE inhibitors (this appeared, partially formed, from the pit of my memory during the wardround. I will check the details and tell all in the next podcast)
MJM
Sunday, January 08, 2006
MP3 File
Reading:
Does this patient have an abnormal venous pressure? Rational clinical examination. Cook DJ. JAMA, 1996;275(8):630pp
Jugular Venous Pulse: an appraisal. Garg N et al. Journal, Indian academy of Clinical medicine. 2000; 1(3):260-269.
Venous Pulse
Wikipedia JVP
Central venous pressure: jugular venous pressure is somewhat helpful.
Subscribe to:
Posts (Atom)